Food Allergies, Eosinophilic Esophagitis (EoE), Autism, Asthma, Celiac Disease and Eczema all have mast cell issues in common. There is a huge need for research into food allergy and its relationship with these other diseases. You have probably heard of most of these diagnoses except for maybe a new diagnosis called Mast Cell Disorder.
My daughter’s and my diagnosis with a Mast Cell Disorder has led me to do some research into mast cell disorders and how they relate to these other diseases, especially since my daughter also has tree pollen allergies, celiac disease and ADHD; I have EoE, environmental and other severe food allergies; and my son has a diagnosis of multiple life threatening food allergies, eczema, environmental allergies and asthma. I believe there’s a huge opportunity to find a cure for these diseases by combining research efforts.
I’ve heard from so many families who have one child with celiac disease and one with food allergies; or some other combination of the issues above that there seems to be a link between these conditions. And as far as I know, no research has been done to look at a ‘main cause’ of all these diagnoses. Yet, all are on the rise in our children.
Additionally, with the Oral Immunotherapy (OIT) and Sublingual Immunotherapy (SLIT) research that’s currently being done in an attempt to find a cure for food allergies, it concerns me greatly that children participating in a research study may not be aware that they might be trading one disease for another. They may be getting rid of their food allergies, and end up being diagnosed with EoE or a mast cell disorder somewhere in their future.
In fact, some children have to cease participation in a research study because of a diagnosis with EoE, that later resolved after ending peanut desensitization. Research on milk OIT was reported at the recent AAAAI meeting where patients were found to become more reactive to milk after three to five years of desensitization. I’m wondering if this is because a threshold has been reached where their immune system has gone into a constant state of reaction – another way of explaining a mast cell disorder.
So much isn’t known about how the immune system functions, and approximately 75% of our immune system is in our gut. It’s quite a gamble in an attempt to find a cure for food allergies!
The Allergic Response
I’m not a medical doctor nor an allergist, but this is what I understand occurs in our body when the body senses an invader, or foreign substance, and the immune system is triggered. An allergy is an overcompensation of the body’s immune system when confronted with the protein of a food, a drug (such as penicillin), a bee sting or an airborne pollen that the body views as an invader. The body releases an overload of histamines in response to the attacker substance, which can create symptoms such as a runny nose all the way to the extreme of anaphylaxis.
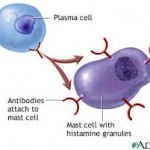
The immune system normally protects the body from harmful items such as bacteria or viruses. In the case of allergies, the immune system has a hypersensitivity or an allergic reaction. During an exposure to an allergen, B cells are alerted and turned into plasma cells which produce IgE (immunoglobulin E) antibodies to fight the “invader.” These antibodies travel through the body until they come into contact with the immune cells called mast cells.
Mast cells are present in the skin, respiratory system and the gut and are important to keep us healthy by fighting off viruses, etc. The antibodies attach themselves to the mast cells via a receptor on the surface and remain attached. That way the next time the immune system meets up with the same invader, the system is primed to react again.
Eosinophils are white blood cells that are one of the immune system components responsible for combating parasites and certain infections. IgE, mast cells, basophils, and eosinophils are essential components of allergic inflammation. Mast cells are tissue resident cells and uniquely required for immediate hypersensitivity. Basophils are largely circulating cells, but home to areas of allergic inflammation during the late phase response. Eosinophils are resident to the GI tract, but also home to allergic inflammatory sites.
Patients with EoE have a high level of white blood cells, or eosinophils, in their esophagus. Research has shown the relationship between high eosinophils and high mast cells. Dr. T. C. Theoharides of Tufts University has found that children with autism have high mast cells, which he postulates causes the severe form of “brain fog” that these patients experience. The brain-blood barrier is compromised and affected by high mast cells. Research has found that patients with untreated Celiac disease have depressed levels of mast cells, as do patients with eczema in different recent research.
Patients with mast cell disorders may or may not have true IgE food allergies; however most of these patients are triggered by high histamine foods. Many are triggered by pollen allergies, and/or certain drugs that increase mast cells. Some, like myself, are so sensitive that food dyes in medications can cause a reaction. It’s interesting that all of these conditions involve mast cells not being “normal.”
A Little History
Since my diagnosis of a mast cell disorder in 2010, I realized how long I have suffered from other allergic issues. I had severe environmental and pollen allergies as a child; got diagnosed with several food allergies in 1993, three years after my daughter was born; and continued to have more and more stomach aches after my son was born in 1996. I got stung by a wasp in 2006, which put my body ‘over the threshold.’
It took 4 years before I got a diagnosis of a Mast Cell Disorder from Dr. Philip Miner, a gastroenterologist with the Oklahoma Foundation for Digestive Research in Oklahoma City, OK. I later found out that Dr. Miner has been researching mast cell disorders since 1988, and only recently has his work been incorporated into medical literature. More and more patients are being diagnosed with mast cell disorders since Dr. Miner has developed the various criteria to review. There are only a few research centers in the USA that have knowledge about mast cell disorders. You can find a listing of these here. Dr. Miner has trained several of these physicians. He is the ultimate researcher, and tells his patients to ‘never give up hope’ that he can help you feel better.
Mast Cell Disorders
You may have heard of systemic mastocytosis or urticaria pigmentosa (also called cutaneous mastocytosis); however Dr. Miner found that there is a spectrum of mast cell disorders that don’t necessarily biopsy in the bone marrow or the skin. One can have a pooling of mast cells in any organ, and my daughter and I have such a pooling in our gut. Patients diagnosed with systemic mastocytosis or urticaria pigmentosa also frequently have stomach aches, since the high mast cell count is not only in their bone marrow or skin, but also frequently found in their stomach.
I’ve learned from Dr. Miner that those of us with mast cell issues have a threshold over which we begin to react. This is true with most of the allergic issues. A high pollen day along with a virus can send your child’s immune system over the edge to where they break out in hives for no apparent reason. Yet what’s really going on is an onslaught of mast cell activity that has made it appear that your child can no longer tolerate certain foods, for example. Or it appears they are having inhalant reactions; or suffering from stomach aches during the Spring and Fall when pollen season is high. Too many mast cells in the body react, and the child goes over a threshold, and begins to react to virtually everything.
The high mast cells in our gut affect the mucosal barrier in our stomach and intestines leading us to ‘leaky gut’ syndrome. This allows even more food proteins to pass into our blood stream causing more food allergies and more reactive issues. My daughter’s leaky gut was exacerbated/created by her celiac disease which she had for 10 years prior to a diagnosis.
The immune system threshold may be reached by a virus, a fragrance, pollen in the air, a drug or a high histamine food. If a patient with a mast cell disorder is skin prick tested or blood tested for an allergy, there may not be a true IgE allergy to the “invader.” The mast cells are just twitchy and ready to react to anything and everything. These reactions can be in the form of hives, stomach aches or life threatening anaphylaxis.
Patients with mast cell issues may be diagnosed with celiac disease yet find their stomach aches continue even on a gluten-free diet. Or the patient may be diagnosed with Irritable Bowel Syndrome, without any biopsy completed to check for high mast cells in the stomach or intestines. Information about mast cell issues is not in abundance on the Internet. Some information about Mast Cell Disease can be found at www.tmsforacure.org and emergency care can be found here.
Published research can be found here. Most of this information is about the systemic form of the disease.
Mast Cells, Histamines, Drugs and Foods
If you believe that you and/or your child is having some mast cell issues and going ‘over the threshold’ on a regular basis, what can you do? Dr. Miner has stated that there are 7 deadly sins for mast cell patients to eat: beef, pork, onions, tomatoes, wheat, oranges, and chocolate. These foods are all high in histamine and his research has shown that mast cell patients can clear up a lot of stomach issues by ceasing to eat these foods. If your child is suddenly “over their threshold” and seemingly reacting to everything, try removing these foods from their diet and see if their system calms down.
Additionally, bananas hold histamine in the body. You may not have an allergy to them, but can still experience symptoms, like hives, if you eat them.
My daughter and I are currently on a very limited diet of foods to try to calm down our mast cell activity. We eat completely organic currently and it’s working! We never had to go on a feeding tube (which many mast cell patients have to do to give their gut a rest), for which we are very grateful. It’s really hard to eat very few foods every day diligently. But constant stomach aches and hives are no fun, so there’s a lot of willingness that we both have to feel better.
If you remove preservatives, GMOs, food dyes and packaged foods from your child’s diet – even if you don’t go completely organic – you might find that your child begins to feel better. That has been our experience.
There are certain drugs that also increase mast cell degranulation. They are:
Aspirin
NSAID’s (Ibuprofen, Motrin, Aleve)
Morphine
Iodine
d-tubocurarine (used in anesthesia)
polymixins (in over the counter bacitracin)
decamethonium
alcohol (if it makes symptoms worse)
Taking even one Ibuprofen pill can affect my stomach. I’ve learned a lot of other ways to get pain relief for muscle aches!
Mast Cell Drug Regimen
There is a drug regimen that is necessary to stabilize the mast cell. Zyrtec and Zantac are used for H1 and H2 histamine blockers. Additionally, to stabilize the mast cell, Gastrocrom (Cromolyn Sodium) is often prescribed, but neither my daughter nor I could tolerate this. Instead, we are on Ketotifen in pill form, which we obtain from a compounding pharmacy since it isn’t formally FDA approved in the USA. Patients may also benefit from Budesonide, a corticosteroid, especially if EoE is also diagnosed.
For those of you with children diagnosed with EoE, you probably notice that many of these drugs are also prescribed to manage Eosinophilic Esophagitis.
In order for mast cell patients to get better, their food, drugs and environment all need to be managed. If a patient is constantly ‘bumping up’ to their threshold, the immune system is constantly firing. And likely they are miserable with stomach aches, nausea, hives, nasal congestion, etc. Eating a low histamine diet, taking all prescribed medications, and watching for individual triggers are necessary to begin the long road to feeling better.
Mast cell disorders are a chronic disorder, and one that will not be outgrown. A patient can go into remission, but it’s very difficult to get to that point if you have been suffering for years with a high mast cell count. It can take months and even years for mast cells in the gut to normalize.
Food Allergy Research & Mast Cells
I have read a lot about the research utilizing Oral Immunotherapy (OIT) and Sublingual Immunotherapy (SLIT) for a cure to food allergies. These desensitization protocols concern me greatly because of the mast cell involvement with food allergies. I’ve yet to see one research study wherein patients are first put through a biopsy of their esophagus, stomach and intestines to get a baseline of their mast cell count at the onset of the study. In my mind, this would give researchers a better idea of which patients are more likely to go over their threshold if their gut mast cell count is already high. I have queried this idea with a leading food allergy research doctor in the USA. His response was that it’s so difficult to get patients to enter into research trials, that asking for a child to have an endoscopy would likely have more parents decline to participate.
Ingesting small amounts of allergens is certain to increase the mast cell count in the gut, and the result could be mast cell issues in years to come. We just don’t have enough research to know what is going to happen to these study participants 10 or 20 years down the road. I say this because of the history of what has happened to me. A child with multiple food allergies may not be able to eat 4 or 5 foods. An adult with a mast cell disorder may only be able to eat 4 or 5 foods!
I receive dozens of emails from families whose children have been diagnosed with EoE, yet most have never heard of a possible mast cell involvement with their child’s EoE. Some GI docs are doing biopsies for mast cells in addition to eosinophils, yet they aren’t using the Alcian Blue 3 stain, which is the only staining that effectively picks up the true level of mast cells according to Dr. Miner. So the GI doc isn’t getting the correct information to properly diagnose the problem.
I’ve also had many discussions with parents who believe that their children have an inhalant allergy to a food. They tell me these stories that are heart wrenching about their children suddenly reacting to peanuts on someone’s breath or something similar. The reactions are frequently quite severe. Inevitably, years down the road I hear from the parent that the child has been diagnosed with EoE. This makes sense in light of the mast cell involvement. If a child has a diagnosed food allergy to peanuts, for example, that may be only part of the story. The child may also have a high mast cell count that manifests into a diagnosis of EoE. Wouldn’t it be nice if the allergist who hears a story of a child having inhalant food reactions could/would send the child to a GI doc for a mast cell disorder check up?
I wish there was more shared research on these various disorders so that children wouldn’t have to suffer needlessly without a proper diagnosis. There is still so much to learn, but I hope that my diagnosis with a mast cell disorder might help others who are suffering recognize some similar symptoms and get help!
I wish that we knew more about the workings of the immune system so that not only could we find a cure for food allergies, but also a cure for EoE, mast cell disorders, autism – the list goes on and on.
I wish that the research of all these conditions were more easily shared with all the various doctors (allergists, pediatricians, GI docs) so that patients didn’t suffer for years before getting a diagnosis.
In the meantime, our family is going to be cautious about what we eat to ensure that we do our part to cease adding diagnoses to our long list!
Read my daughter’s story of mast cell issues here.
You can also read all of the mast cell & Eosinophil blog posts here.
Hi — Thank you for the information on this site. I must admit I’ve rushed through what’s on this page and haven’t had time to fully digest it, but am bookmarking it for later browsing. My 13-year-old twins have had asthma and allergy issues as long as I can remember, but recently my son has “developed” (?) allergies to latex, cosmetic preservatives in the last year, and — we just discovered — cold. That last one is scaring me to death (he broke out twice in full-body hives and we are so lucky it didn’t result in shock…) He was already allergic to peanuts, furry animals, mold, pollens — and he seems to be becoming more reactive as time goes by. I was lucky enough to have joined an latex allergy discussion forum and asked if anyone knew anything about cold urticaria — and a few people there suggested that we look into mast cell disorders. It certainly makes more sense that there is something wrong with the way his body reacts than it does to assume that he’s acquiring new and improved allergies — and attempting to treat them individually. I spent yesterday writing letters to my son’s pediatrician and allergist asking if a mast cell disorder could be investigated (and documented the letter with photographs of a home “cold urticaria test” we performed with ice cubes and a clock :)) and am hoping this will get the ball rolling in the right direction. And am hoping we can speed things up and avoid a consult or two spent trying to get the parents to calm down and stop diagnosing their kid via the internet… 🙂 Thank you and I’m looking forward to learning more. Monica
Good luck Monica. Keep us updated with what you find out!
Nicole — I have no idea if you’ll see this post (3 years later), but I was fascinated to stumble back onto this site (I had forgotten even posting the above description of my son’s allergy issues) — but since then my son was diagnosed last April with Eosinophilic Gastroenteritis. We’ve struggled for the last year with steriods, elimination diets, etc. — and I am absolutely convinced this is not a food issues (solely) but a tipping point issue. (His symptoms began in Spring 2015 after a horrible pertussis-like few months of coughing, an injection he seemed to react to, and what I can only assume were already aggravated reactions from elevated mold and pollen levels.) His GI symptoms definitely seem to fluctuate seasonally. I’m currently butting heads with his GI and Allergy docs (they’re convinced a food item or two is the cause) — and am pursuing getting him seen by a doc in NC that has diagnosed at least one other patient with eosinophilic symptoms with a mast cell disorder. (I can’t get his current doctors to look outside their in-the-box EOE treatments.) I’m desperate to see if I can get him better without steriods… Thank you again for the information. Monica
I sent you an email directly Monica!
Hi – Thank you for this fascinating information. My 7 year old son has a long and growing list of allergies also. Tree nuts, wasps, mold, dust, cats, horses, as well as asthma. You mention your concerns surrounding immunotherapy. Interestingly, my son started venom immunotherapy for his wasp allergy last year, and he has since developed stomach issues that have, so far, been undiagnosable. I don’t even know where to begin though to try to investigate the possibility of a mast cell disorder.
Jen – Ottawa, Canada
Jen – You might want to check out The Mastocytosis Society website: http://www.tmsforacure.org to find a mast cell research center near you.
Thank you so much for your post; it helped a lot to read it, especially right now. My family is currently waiting on tenterhooks for the results for my daughter’s test for Mast cell activation disorder. We should know any day now.
My 15 year old daughter is also a celiac (me too), with gut pain that never stops, gets worse with many, many foods (like chocolate and onions), and has been slowly growing worse over the last few years. She has environmental allergies but tests negative for all other allergens.
And all her tests come back as fine, no problems…it must all be anxiety, all in her head. My keeping her away from foods, dyes, preservatives and such that cause so much gut pain she stops eating? That’s all in my head. 😛
I was diagnosed with MCAD just a few weeks ago and immediately scheduled her for an appointment to see if the doctor felt it would be worth testing her for this, too. I do not know if a mast cell disorder is what she has, but we’re both hoping and dreading a diagnosis. We desperately want an answer, but I would love it if it could be a less debilitating one, you know?
Again, thank you for sharing this. It helped to read of others going through some similar situations and making it through. 🙂
May I ask which doctor you found to diagnose the MCAD? I’ve heard from so many people about their problems finding a doctor who can accurate diagnose this debilitating illness!
No problem. ^_^ A Dr. Tara Carr at the University of Arizona Medical Center. She diagnosed me, she was willing to test my teenaged daughter for the same thing, and I know of another teen who came to see her recently with similar symptoms (I told the mother about her) and she is testing that boy for MCAD and Masto, as well. So it’s definitely not a one time thing.
On the negative side, when I was diagnosed, I asked if she had any information on it to give me on it and she had nothing except an article that she went to go copy from a previous patient. But not even the name of a support group, unfortunately (although there turned out to be one at the bottom of the article). Not a lot of advice in the beginning aside from starting me on trying to find an anti-histamine that worked, nothing talking about drug precautions, keeping a trigger journal, none of that. I am going to see her for a follow-up in another month, but it still felt a bit like being tossed to the wolves after being diagnosed, you know?
However, she took one look at my history, did a quick prick test of some allergens, and then MCAD and Mastocytosis were the next things she looked at, ordering the tests that first appointment. So while she didn’t have a lot of support, she did very well on identification. From that perspective, she was still miles above most specialists I’ve had to see. The entire southwest USA seems to be kind of the MCAD wasteland when it comes to doctors!
I know what you mean about the problems with finding a good doctor. A few of us started a facebook support group – AZ Mast Cell Support – and sharing which doctors we found and how they are doing is one of the first thing everyone wanted to do!
Thanks for the info. I’ve had a gentleman from Phoenix contact me recently about mast cells, so I’ll let him know!
Awesome!
Thank you!
Do you know if NAET is harmful to mast cell count? I am currently having treatments, because I am at my wits’ end trying to figure out why I am suddenly reacting to everything around me… and only just came across Mast cell activation disorder the other day. Wondering if it’s worth continuing NAET or if I should look into Mast cell issues instead.
The only thing that NAET did for me was to lighten my wallet! I’d suggest looking into mast cell issues instead.
My children have been doing that since BIRTH! I forced my husband to pay attention to the foods they refused when they were infants and toddlers. It was ALWAYS foods that were likely to make them ILL if they had the same diseases and diagnoses I had, but hadn’t been seen for yet.
When I’d put ANYTHING with dairy (organic and grass fed only!) they showed AVERSION to it. Crinkled their noses and face and raspberried at the foods in front of them…and they NEVER put it in their mouth!
Did it to dairy, bananas, CHOCOLATE (I seriously don’t know if I am going to be able to live without this…), most yeast risen gluten ridden bread…even when I am baking or cooking it MYSELF (I’m a food blogger), ANY red meat, pork, anything pickled, any nuts…but ESPECIALLY peanuts, all condiments, coconut, cinnamon, nutmeg, cumin, chickpeas, heavy poultries (like goose, duck, or pheasant), stone fruits, berries, soda (now….I did NOT offer this to them, my FATHER IN LAW did, and I was STUNNED at the idiocy of it but….as soon as it got near their noses they raspberried at it and….gratefully grandpa decided they wouldn’t like it. Man, was I pissed off when he did that!), most olives, onions, etc
I mean…we’re down to eggs, pears, cilantro, basil, turkey, chicken, rice…the list of what we CAN eat without stomach upset, nausea, gastrointestinal involvement, etc…it is VERY short. I have chiari, syringomyelia, degenerative disk disease, spinal stenosis, fibromyalgia, EDS (they aren’t sure what type yet, and my Sx have crossover but I have the MOST symptoms for hEDS and vEDS…veins roll, BLOW from vaccutane tubes, etc), POTS, MCAD, and NOW scoliosis (I didn’t have scoliosis my ENTIRE life…after being decompressed and NOT being aware that I had EDS and wasn’t on the Cusack Protocol has caused the result of my decompression surgery to FAIL. I had a full spine, brain, and cine flow done in 2015 with and Wout contrast (which I ALSO react to…never a day off!) and there was NO scoliosis, I was 35 when they did that. A year later in August of 2016 I was having sharp, CONSTANT pain in my lower left back and NO physician could figure out what was happening. The pain began in my lumbar but if I couldn’t get a handle on it quick enough, it began to migrate to INCLUDE my entire spine and HEAD. All the doctors heard was “head” and “I’ve been decompressed..” and they did CTs on my head and ABDOMEN lol and didn’t actually x ray my back! I ended up in a kinesiologist chiropractor’s office bawling because I JUST wanted the pain to STOP. An ER doc had given me 1mg of dilaudid and it didn’t TOUCH the pain. The chiropractor did a full series of x ray of my entire spine and head and was going over the results with me. He was in the middle of explaining what he found that I had already told him about so…he was telling me “…here’s the degenerative disks you were talking about all along your spine, it seems pretty advanced so I imagine you didn’t look like this at 23 when they first told you about your DDD and your C2/C3 fusion. Then here we see the start of what looks to ME like spinal stenosis, and it goes all the way down to your arthritic sacrum that you told me about, and it MIGHT be what is irritating your scoliosis and your….” and I interrupted hiim…”SCOLIOSIS…what?!” Things devolved from there. I just started sobbing. In less than 1 calendar year between my 35th and 36th birthday, I popped scoliosis in my lumbar. It was NEVER there before and….NO doctor could tell me HOW that could happen. But…ALL of my fellow chiari support groups (five of them including peds groups) gave me the SAME exact causation. Ehlers-Danlos Syndrome. They also all said the same thing…”it took you 9 months to get your doctor to order the MRI that found your CM1 and SM and then you were given the WRONG prognosis for future care. Sorry to tell you…what LITTLE most neurosurgeons and neurologists know about chiari malformation is WAY more than MOST doctors know about EDS. Getting an EDS diagnosis can take, on average, 8 YEARS.” I just wanted to go out into the woods like a DOG does when it knows it is dying, pick a good view, and…go lol EVERY doctor I mention “scoliosis post decompression is evidence of an underlying connective tissue disorder, namely Ehlers-Danlos Syndrome…most likely hypermobility type, that wasn’t found BEFORE decompression.” spreads a look across their face of either incredulity or flat out skepticism…then denial. I can’t tell you how LONG my diagnoses and my children’s have been to get documented because a physician either REFUSES the TESTS needed to diagnose it or says I am WRONG about causation. Because THEY aren’t familiar with the research, my children and I suffer. It is a highly DELICATE process to present information, act like I’m “not sure” if it has anything to do with my Sxs, but…then fill in the blank with a way for THEM to make the connection in THEIR head on their own, so I don’t have to hold their hand TO it. I end up having to somehow make it seem like THEY discovered the relevant information instead of ME. If there is ego ANYwhere in the exam room…I’m not going to get the help I need. If they haven’t been keeping up with their REQUIRED 50-75 continuing education credit hours….I leave right where I walked in. Nowhere.) on top of it all.
I just saw a doctor for the MCAD yesterday and he ordered lab work but…every time I talk to our pediatrician about MCAD she said that our youngest WAS tested for it when he was born but…I don’t want to piss her off by telling her that an MCAD test on a NEWBORN is NOT going to pop positive for a problem. Heel sticks happen sometimes minutes or HOURS after being born. WHAT THE HELL are they going to have had PUT INTO them that was going to make their mast cells reactive at that point???!! Right. NOTHING. So….with my MCAD comes CHRONIC, severe insomnia. I use my time to read scholarly STUDIES all night. It is ALARMING how long some of the information on my diseases, comorbidities, and causation correlations have been KNOWN, but the physicians know NOTHING about those studies or connections. The study that linked regressive result to CM1 craniotomy with laminectomy was written in 2007! It has been known for 10 YEARS….chiari patients know it, but my neurosurgeon here at this base and at the base we were at in Oklahoma when the chiari was found…he has NO idea. He also told me decompression wouldn’t be a good idea for me. He insisted it is a last resort, but ONLY when you get to the point that you’re crapping your pants, etc. And yes…he actually SAID that. Until there are life threatening or SEVERE quality of life issues happening…decompression isn’t warranted. That medical opinion bothered me greatly. He used another patient of his…a woman in her mid 30s with 5 children who has now SO much nerve damage that she’s incontinent, that is someone who should be decompressed. I looked him in the face and asked him if he KNEW he was wrong or if he is just AFRAID to operate on me, and he kicked me out of his office. These are the doctors my children and I have to depend on for my care.
So, I went and READ some studies, and decided to look for a second opinion. My second opinion disagreed with the first opinion. He said what I suspected which was…if I let this go when there is only MINOR (in his estimation based on what he’s seen in the end stages of life with someone who has CM1) issues, the nerve damage and decline of my health will be much faster than I’d want it to be. Based on lifestyle and age he gave me a 70% chance of resolve of most of my symptoms. We were shipping to an overseas assignment less than a year later, and the neurosurgeon I was assigned to agreed with Dr. Second Opinion. So I was decompressed as fast as they could do it. I woke up to ZERO pain for the FIRST time in my life, and then realized how SEVERE the pain I’d been living with my entire life really had been. My result only lasted about 3 years before I was havinga recurrence in pain but the 2015 MRIs showed NO reason for it. This is where the MCAD, EDS, POTS journey began. And it has been HELL. =(
Do you know what I am doing today?? Cheek swab for drug resistance testing. I am not going to be diagnosed on paper with 3 diseases I KNOW I have before the Air Force moves us next year (they move us every 3 years….it isn’t pleasant.) and EVERY single time they move us…I start over. Every doctor has to feel like Christopher Columbus about your body. They don’t take other physicians WORD for it and they end up repeating the same tests I already had, and the WORST part is, if something about my condition improved even SLIGHTLY, they won’t find the lab confirmations that I’d need for them to move in the direction I was already headed in before I was assigned to them as a patient.
These behaviors in the medical community KILL people. The NEW medical negligence is NOT examining the patient at ALL. Malpractice and negligence USED TO BE cutting off the wrong hand, KNOWING a patient had a disease and ignoring it or MISdiagnosing a patient with a lesser disease than what they had and then the patient died from lack of treatment. Today, medical malpractice is usually not even POSSIBLE because BEFORE an initial consultation, your doctor will send a referral and any supporting medical necessity information. But 2 things happen….the doctor who is sending you is sending you because they lack the expertise on THAT body system, so the likelihood that they send ALL of the information the specialists needs is quite low. If they do send paperwork and it is incomplete or not good enough you’ll get a phone call from the specialists office saying “Dr. Soandso has declined to evaluate you. He looked at the supporting documentation your primary care doctor sent, and he doesn’t feel that he can add anything to the situation at this time. Thank you… *click*” OR the primary care doc DOES send everything and you get in the door BUT…the doctor you were sent to got his MD in the 70s and has NOT bothered to keep abreast of research and new findings so when you’re in say…a dermatologist’s office and ask for a biopsy to diagnose EDS the white haired man looks at you as if he is confused and says “What makes you THINK you have Ehlers-Danlos Syndrome…. Hold our your arms…” and he proceeds to try to do the Beighton on you at almost 37 years old, because he doesn’t know the NEW hypermobility major and minor criteria for clinical diagnosis AND…the only EDS type he’s familiarized himself with tells HIM, he has to be looking at a GUMBY to diagnose it. Then….when you tell him “there are about 13-16 different types of EDS. The one we’re most concerned about is vascular EDS…” He interrupts you and says “…what’s vascular EDS…?” At that point the 2 residents in the room (students who are trying to LEARN) are looking at the floor because he’s talking DOWN to the patient, treating the patient like a MORON in front of their spouse, and then…WITH NO EXAM WHATSOEVER, JUST LOOKING AT YOU…he announces that you’re EDS FREE. When he notices you’re starting to cry (because you look horrible in ORANGE, and jumpsuits… But most of all, the PTSD from doctors CONSTANTLY telling you there is NOTHING wrong with you when there REALLY is…very SERIOUS conditions and you KNOW it… It eventually BREAKS you.) he softens his voice a TAD and touches your shoulder while he says “…hey, no this is a GOOD thing. You don’t have EDS. There isn’t a CURE for that, so…me telling you that you don’t have it is GOOD.” and walks OUT…and that is what you relay to your primary care doctor, while she is busy looking SHOCKED that someone would do that. You get sent to a SECOND dermatologist who has basically been ordered by your primary care doctor to LOB OFF SKIN for a biopsy, whether you THINK the patient is sick or NOT. The dermatologist complies, but sends your skin to the gene facility with NO paperwork or order for a test. So…they have to call the doctor to ask, then fax the order to the derm doc and the doc chooses a Marfan panel instead of the Heritable Disorders of Connective Tissue panel that looks for 16 EDS proteins rather than just FOUR which is the Marfan panel….you KNOW you’ve just been screwed. On top of it, thanks to the EDS everyone is telling you that you DON’T have, your non existent immune system doesn’t kick in to HEAL that biopsy site where 2 stitches were put. Instead, it does what you told the derm doc it WOULD do, it gives you cellulitis. Because you KNEW this would happen…you asked her for Keflex WHILE she was still in the exam room tubing up your skin, but she chuckles and says “Oh, you’ll be fine. No worries!” and leaves…you get a little worried. As per usual…you ended up knowing the body YOU have had for over 30 years…and you have a NASTY cellulitis infection in LESS than 48 hours. You have to track down the derm doc through her answering service on a Friday at 5pm to get your keflex. Even being on it for the 2 weeks doesn’t completely KILL the cellulitis…less than 24 hours after completing the keflex…the cellulitis is coming BACK. After 5 weeks. you call the gene facility to see if the results are in…not yet. But 3 days later you get a call from the derm doc’s office telling you that you’re “EDS free…”, but your GUT tells you…no, that can’t be right. That’s when you find out ALL of the fabulous flubs the doc made in the sending and ordering, and the facility TELLS YOU the derm doc ordered the wrong test, and that the derm doc CANNOT use their facility’s name to say that THEY pronounced me EDS free…a genetic counselor from the facility tries to contact your primary care doctor, because they hold onto your skin for 6 months…and after cellulitis you’re GRATEFUL for that but…in the same call you find out the derm doc COULD HAVE just SENT BLOOD. @.@ After 2 weeks of trying to finesse the derm doc into testing the other panel, she announces that she’s no longer my doctor of service, thank you very much…goodbye.
The worse part about the WHOLE thing is…her little office staff people said..”we order these tests ALL OF THE TIME for people to diagnose their EDS…” and you realize…there are probably THOUSANDS of people walking around your town who DO have EDS but don’t know the derm doc did that. They keep trying to refer you to a geneticist that NO longer accepts patients because he is moving his practice to Kansas City lol but he is the ONLY geneticist in TOWN that sees ADULTS for EDS.
You really…start feeling QUITE hopeless because you know you have the symptoms of these diseases but, NO ONE is looking for ways to confirm it OR rule it out PROPERLY. You feel like giving up.
That is the NEW medical negligence. Deny there is a problem, refuse to test, refuse to treat, refuse to even examine… That is 2017. When EVERY hospital has multiple MRI and CT machines, x rays are DIGITAL and radiologists can instantly interpret the images, gene testing can find genetic markers that are present in people with a high inclination to get CERTAIN TYPES of CANCER…WHOLE FACES are being transplanted, and a WHOLE HEAD is about to be put on a new body somewhere in Russia…but…. I can’t get a doctor to properly examine me for EDS and…it IS going to kill me. I am trying to not let that happen and I am failing. This is as much for my children and husband as it is for me. All 3 of our children have EDS in some form. Our oldest has POTS symptoms with his, our middle has confirmed chiari malformation 1(which took me 2 years and 3 peds docs before they would look.), our youngest has EDS…and it looks to be the vascular kind and he is our MOST obvious MCAD child. My husband…also has EDS with scoliosis and he didn’t know that his hypermobility was part of a HUGE systemic disease. I also believe he has chiari but…NO MRI. They WON’T do it.
I can’t handle that in 2017 those ^^^^^^^^ things are STILL happening to people. Science has advanced SO much, but…not very many people are USING it. It is astonishing. And terrifying all at the same time.