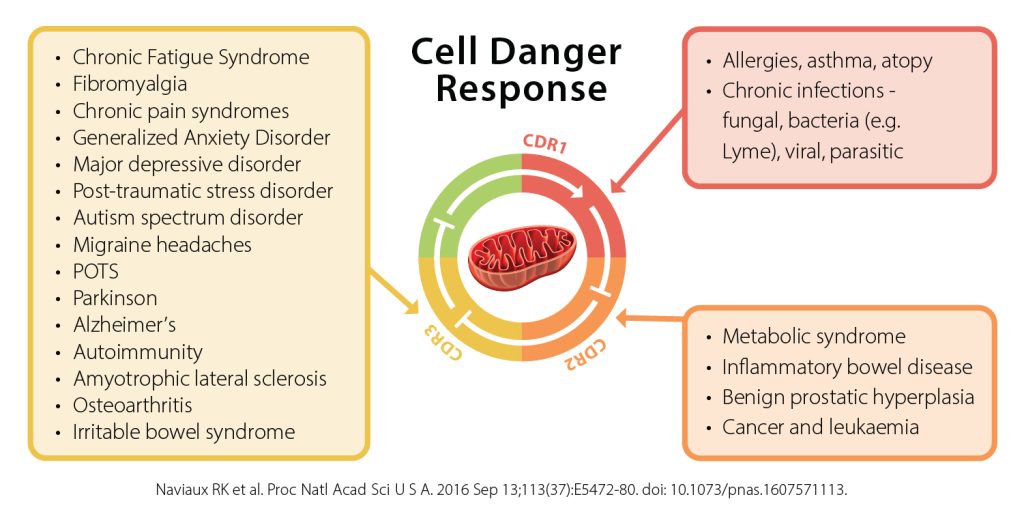
Food Allergies, Eosinophilic Esophagitis (EoE), Autism, Asthma, Celiac Disease and Eczema all have mast cell issues in common. There is a huge need for research into food allergy and its relationship with these other diseases. You have probably heard of most of these diagnoses except for maybe a new diagnosis called Mast Cell Disorder.
My daughter’s and my diagnosis with a Mast Cell Disorder has led me to do some research into mast cell disorders and how they relate to these other diseases, especially since my daughter also has tree pollen allergies, celiac disease and ADHD; I have EoE, environmental and other severe food allergies; and my son has a diagnosis of multiple life threatening food allergies, eczema, environmental allergies and asthma. I believe there’s a huge opportunity to find a cure for these diseases by combining research efforts.
I’ve heard from so many families who have one child with celiac disease and one with food allergies; or some other combination of the issues above that there seems to be a link between these conditions. And as far as I know, no research has been done to look at a ‘main cause’ of all these diagnoses. Yet, all are on the rise in our children.
Additionally, with the Oral Immunotherapy (OIT) and Sublingual Immunotherapy (SLIT) research that’s currently being done in an attempt to find a cure for food allergies, it concerns me greatly that children participating in a research study may not be aware that they might be trading one disease for another. They may be getting rid of their food allergies, and end up being diagnosed with EoE or a mast cell disorder somewhere in their future.
In fact, some children have to cease participation in a research study because of a diagnosis with EoE, that later resolved after ending peanut desensitization. Research on milk OIT was reported at the recent AAAAI meeting where patients were found to become more reactive to milk after three to five years of desensitization. I’m wondering if this is because a threshold has been reached where their immune system has gone into a constant state of reaction – another way of explaining a mast cell disorder.
So much isn’t known about how the immune system functions, and approximately 75% of our immune system is in our gut. It’s quite a gamble in an attempt to find a cure for food allergies!
The Allergic Response
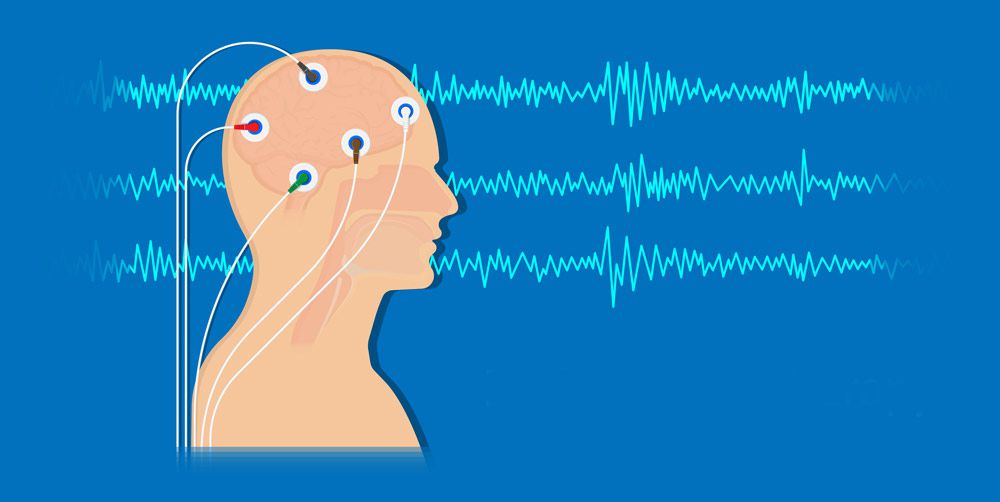
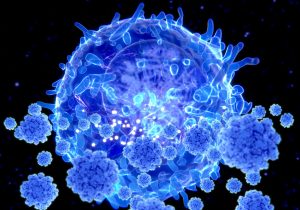
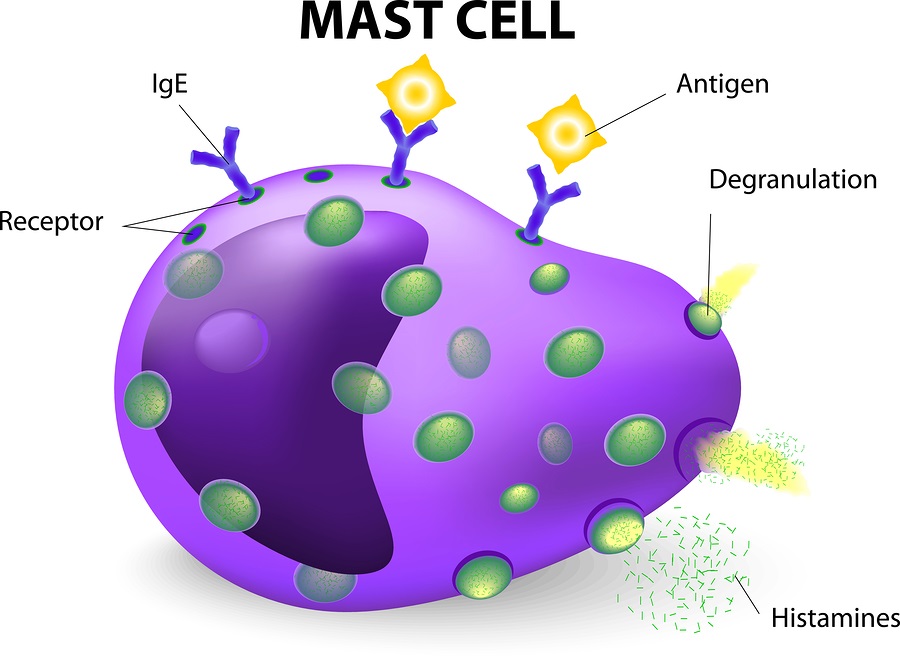
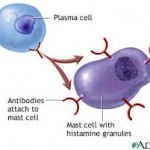
I’m not a medical doctor nor an allergist, but this is what I understand occurs in our body when the body senses an invader, or foreign substance, and the immune system is triggered. An allergy is an overcompensation of the body’s immune system when confronted with the protein of a food, a drug (such as penicillin), a bee sting or an airborne pollen that the body views as an invader. The body releases an overload of histamines in response to the attacker substance, which can create symptoms such as a runny nose all the way to the extreme of anaphylaxis.
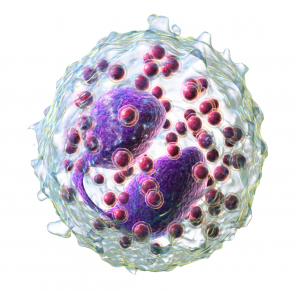
The immune system normally protects the body from harmful items such as bacteria or viruses. In the case of allergies, the immune system has a hypersensitivity or an allergic reaction. During an exposure to an allergen, B cells are alerted and turned into plasma cells which produce IgE (immunoglobulin E) antibodies to fight the “invader.” These antibodies travel through the body until they come into contact with the immune cells called mast cells.
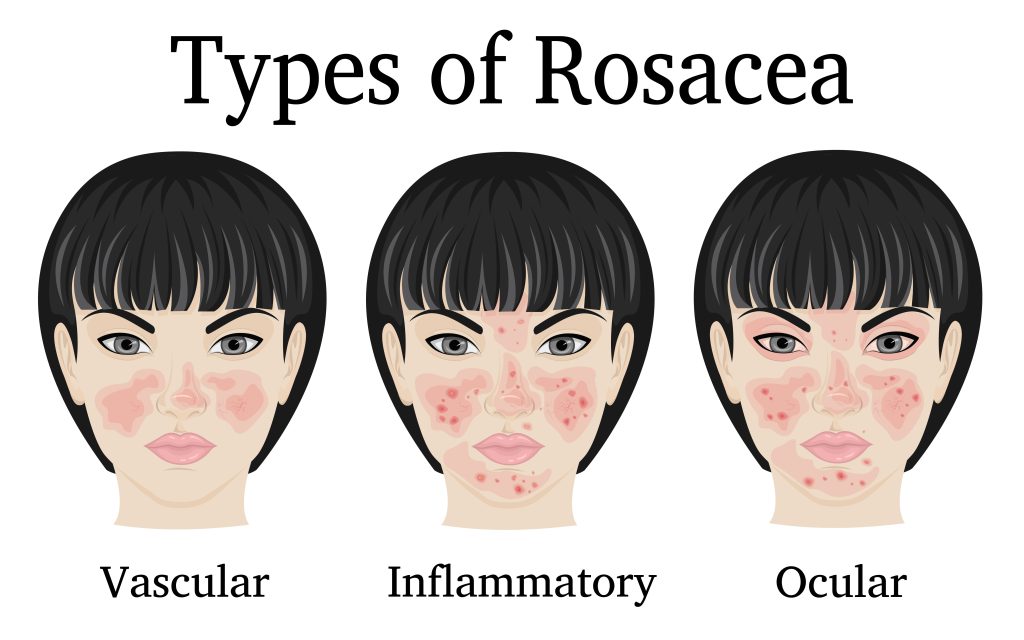
Mast cells are present in the skin, respiratory system and the gut and are important to keep us healthy by fighting off viruses, etc. The antibodies attach themselves to the mast cells via a receptor on the surface and remain attached. That way the next time the immune system meets up with the same invader, the system is primed to react again.
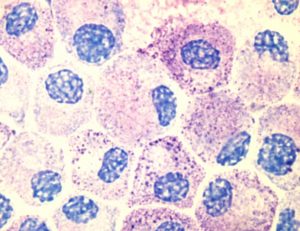
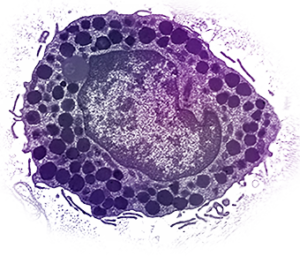
Eosinophils are white blood cells that are one of the immune system components responsible for combating parasites and certain infections. IgE, mast cells, basophils, and eosinophils are essential components of allergic inflammation. Mast cells are tissue resident cells and uniquely required for immediate hypersensitivity. Basophils are largely circulating cells, but home to areas of allergic inflammation during the late phase response. Eosinophils are resident to the GI tract, but also home to allergic inflammatory sites.
Patients with EoE have a high level of white blood cells, or eosinophils, in their esophagus. Research has shown the relationship between high eosinophils and high mast cells. Dr. T. C. Theoharides of Tufts University has found that children with autism have high mast cells, which he postulates causes the severe form of “brain fog” that these patients experience. The brain-blood barrier is compromised and affected by high mast cells. Research has found that patients with untreated Celiac disease have depressed levels of mast cells, as do patients with eczema in different recent research.
Patients with mast cell disorders may or may not have true IgE food allergies; however most of these patients are triggered by high histamine foods. Many are triggered by pollen allergies, and/or certain drugs that increase mast cells. Some, like myself, are so sensitive that food dyes in medications can cause a reaction. It’s interesting that all of these conditions involve mast cells not being “normal.”
A Little History
Since my diagnosis of a mast cell disorder in 2010, I realized how long I have suffered from other allergic issues. I had severe environmental and pollen allergies as a child; got diagnosed with several food allergies in 1993, three years after my daughter was born; and continued to have more and more stomach aches after my son was born in 1996. I got stung by a wasp in 2006, which put my body ‘over the threshold.’
It took 4 years before I got a diagnosis of a Mast Cell Disorder from Dr. Philip Miner, a gastroenterologist with the Oklahoma Foundation for Digestive Research in Oklahoma City, OK. I later found out that Dr. Miner has been researching mast cell disorders since 1988, and only recently has his work been incorporated into medical literature. More and more patients are being diagnosed with mast cell disorders since Dr. Miner has developed the various criteria to review. There are only a few research centers in the USA that have knowledge about mast cell disorders. You can find a listing of these here. Dr. Miner has trained several of these physicians. He is the ultimate researcher, and tells his patients to ‘never give up hope’ that he can help you feel better.
Mast Cell Disorders
You may have heard of systemic mastocytosis or urticaria pigmentosa (also called cutaneous mastocytosis); however Dr. Miner found that there is a spectrum of mast cell disorders that don’t necessarily biopsy in the bone marrow or the skin. One can have a pooling of mast cells in any organ, and my daughter and I have such a pooling in our gut. Patients diagnosed with systemic mastocytosis or urticaria pigmentosa also frequently have stomach aches, since the high mast cell count is not only in their bone marrow or skin, but also frequently found in their stomach.
I’ve learned from Dr. Miner that those of us with mast cell issues have a threshold over which we begin to react. This is true with most of the allergic issues. A high pollen day along with a virus can send your child’s immune system over the edge to where they break out in hives for no apparent reason. Yet what’s really going on is an onslaught of mast cell activity that has made it appear that your child can no longer tolerate certain foods, for example. Or it appears they are having inhalant reactions; or suffering from stomach aches during the Spring and Fall when pollen season is high. Too many mast cells in the body react, and the child goes over a threshold, and begins to react to virtually everything.
The high mast cells in our gut affect the mucosal barrier in our stomach and intestines leading us to ‘leaky gut’ syndrome. This allows even more food proteins to pass into our blood stream causing more food allergies and more reactive issues. My daughter’s leaky gut was exacerbated/created by her celiac disease which she had for 10 years prior to a diagnosis.
The immune system threshold may be reached by a virus, a fragrance, pollen in the air, a drug or a high histamine food. If a patient with a mast cell disorder is skin prick tested or blood tested for an allergy, there may not be a true IgE allergy to the “invader.” The mast cells are just twitchy and ready to react to anything and everything. These reactions can be in the form of hives, stomach aches or life threatening anaphylaxis.
Patients with mast cell issues may be diagnosed with celiac disease yet find their stomach aches continue even on a gluten-free diet. Or the patient may be diagnosed with Irritable Bowel Syndrome, without any biopsy completed to check for high mast cells in the stomach or intestines. Information about mast cell issues is not in abundance on the Internet. Some information about Mast Cell Disease can be found at www.tmsforacure.org and emergency care can be found here.
Published research can be found here. Most of this information is about the systemic form of the disease.
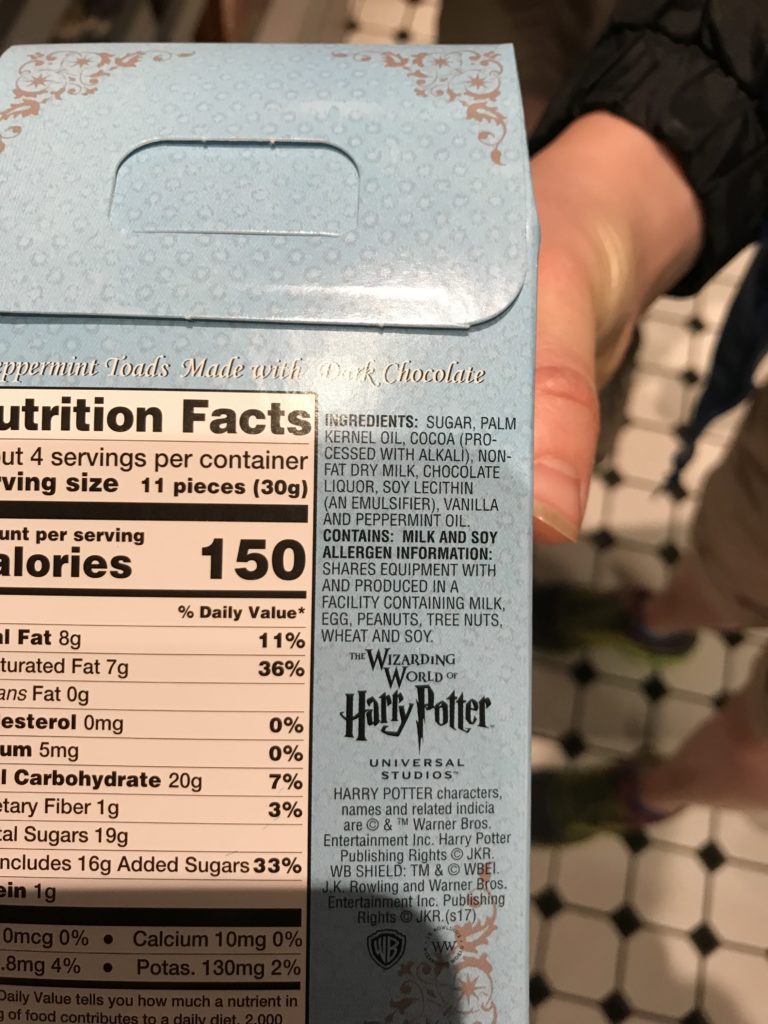
Mast Cells, Histamines, Drugs and Foods
If you believe that you and/or your child is having some mast cell issues and going ‘over the threshold’ on a regular basis, what can you do? Dr. Miner has stated that there are 7 deadly sins for mast cell patients to eat: beef, pork, onions, tomatoes, wheat, oranges, and chocolate. These foods are all high in histamine and his research has shown that mast cell patients can clear up a lot of stomach issues by ceasing to eat these foods. If your child is suddenly “over their threshold” and seemingly reacting to everything, try removing these foods from their diet and see if their system calms down.
Additionally, bananas hold histamine in the body. You may not have an allergy to them, but can still experience symptoms, like hives, if you eat them.
My daughter and I are currently on a very limited diet of foods to try to calm down our mast cell activity. We eat completely organic currently and it’s working! We never had to go on a feeding tube (which many mast cell patients have to do to give their gut a rest), for which we are very grateful. It’s really hard to eat very few foods every day diligently. But constant stomach aches and hives are no fun, so there’s a lot of willingness that we both have to feel better.
If you remove preservatives, GMOs, food dyes and packaged foods from your child’s diet – even if you don’t go completely organic – you might find that your child begins to feel better. That has been our experience.
There are certain drugs that also increase mast cell degranulation. They are:
Aspirin
NSAID’s (Ibuprofen, Motrin, Aleve)
Morphine
Iodine
d-tubocurarine (used in anesthesia)
polymixins (in over the counter bacitracin)
decamethonium
alcohol (if it makes symptoms worse)
Taking even one Ibuprofen pill can affect my stomach. I’ve learned a lot of other ways to get pain relief for muscle aches!
Mast Cell Drug Regimen
There is a drug regimen that is necessary to stabilize the mast cell. Zyrtec and Zantac are used for H1 and H2 histamine blockers. Additionally, to stabilize the mast cell, Gastrocrom (Cromolyn Sodium) is often prescribed, but neither my daughter nor I could tolerate this. Instead, we are on Ketotifen in pill form, which we obtain from a compounding pharmacy since it isn’t formally FDA approved in the USA. Patients may also benefit from Budesonide, a corticosteroid, especially if EoE is also diagnosed.
For those of you with children diagnosed with EoE, you probably notice that many of these drugs are also prescribed to manage Eosinophilic Esophagitis.
In order for mast cell patients to get better, their food, drugs and environment all need to be managed. If a patient is constantly ‘bumping up’ to their threshold, the immune system is constantly firing. And likely they are miserable with stomach aches, nausea, hives, nasal congestion, etc. Eating a low histamine diet, taking all prescribed medications, and watching for individual triggers are necessary to begin the long road to feeling better.
Mast cell disorders are a chronic disorder, and one that will not be outgrown. A patient can go into remission, but it’s very difficult to get to that point if you have been suffering for years with a high mast cell count. It can take months and even years for mast cells in the gut to normalize.
Food Allergy Research & Mast Cells
I have read a lot about the research utilizing Oral Immunotherapy (OIT) and Sublingual Immunotherapy (SLIT) for a cure to food allergies. These desensitization protocols concern me greatly because of the mast cell involvement with food allergies. I’ve yet to see one research study wherein patients are first put through a biopsy of their esophagus, stomach and intestines to get a baseline of their mast cell count at the onset of the study. In my mind, this would give researchers a better idea of which patients are more likely to go over their threshold if their gut mast cell count is already high. I have queried this idea with a leading food allergy research doctor in the USA. His response was that it’s so difficult to get patients to enter into research trials, that asking for a child to have an endoscopy would likely have more parents decline to participate.
Ingesting small amounts of allergens is certain to increase the mast cell count in the gut, and the result could be mast cell issues in years to come. We just don’t have enough research to know what is going to happen to these study participants 10 or 20 years down the road. I say this because of the history of what has happened to me. A child with multiple food allergies may not be able to eat 4 or 5 foods. An adult with a mast cell disorder may only be able to eat 4 or 5 foods!
I receive dozens of emails from families whose children have been diagnosed with EoE, yet most have never heard of a possible mast cell involvement with their child’s EoE. Some GI docs are doing biopsies for mast cells in addition to eosinophils, yet they aren’t using the Alcian Blue 3 stain, which is the only staining that effectively picks up the true level of mast cells according to Dr. Miner. So the GI doc isn’t getting the correct information to properly diagnose the problem.
I’ve also had many discussions with parents who believe that their children have an inhalant allergy to a food. They tell me these stories that are heart wrenching about their children suddenly reacting to peanuts on someone’s breath or something similar. The reactions are frequently quite severe. Inevitably, years down the road I hear from the parent that the child has been diagnosed with EoE. This makes sense in light of the mast cell involvement. If a child has a diagnosed food allergy to peanuts, for example, that may be only part of the story. The child may also have a high mast cell count that manifests into a diagnosis of EoE. Wouldn’t it be nice if the allergist who hears a story of a child having inhalant food reactions could/would send the child to a GI doc for a mast cell disorder check up?
I wish there was more shared research on these various disorders so that children wouldn’t have to suffer needlessly without a proper diagnosis. There is still so much to learn, but I hope that my diagnosis with a mast cell disorder might help others who are suffering recognize some similar symptoms and get help!
I wish that we knew more about the workings of the immune system so that not only could we find a cure for food allergies, but also a cure for EoE, mast cell disorders, autism – the list goes on and on.
I wish that the research of all these conditions were more easily shared with all the various doctors (allergists, pediatricians, GI docs) so that patients didn’t suffer for years before getting a diagnosis.
In the meantime, our family is going to be cautious about what we eat to ensure that we do our part to cease adding diagnoses to our long list!
Read my daughter’s story of mast cell issues here.
You can also read all of the mast cell & Eosinophil blog posts here.